

A researcher who created a test to diagnose oesophageal cancer explains why the disease is on the rise in the UK, as part of an awareness campaign.
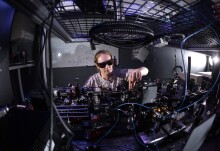
Professor George Hanna is the Director of NIHR-Diagnostic Evidence Cooperative at Imperial College London, and he and his team devised a breath test that can diagnose oesophageal cancer in minutes.
Oesophageal cancer is a form of cancer that affects the pipe that connects the mouth to the top of the stomach. It is the ninth most common type of cancer in the UK, with more than 8,500 new cases diagnosed each year.
February marks the start of Oesophageal Cancer Awareness Month, an initiative led by the charity Action against Heartburn, to encourage people suffering from symptoms such persistent heartburn to visit their GP to check for underlying causes.
As part of Oesophageal Cancer Awareness Month, Maxine Myers caught up with Professor Hanna to find out why cases of this disease are rising in the UK and how his breath test could save lives.
1) Why is oesophageal cancer such a big concern in the UK?
The UK has the highest incidences of oesophageal cancer in Western Europe, with 7,000 people dying each year from the disease. In particular oesophageal adenocarcinoma, a form of the disease, is rising rapidly in men over the age of 60. Like many types of cancer, certain lifestyle factors can increase your risk. For example, the disease is common among people who smoke, drink heavily, are overweight or obese and have a diet low in fruit and veg. People who have long-term persistent heartburn can also be at risk. This is because it can cause chronic inflammation in the cells lining the oesophagus and chemical changes to the DNA inside them. This is known as Barrett’s Oesophagus which can lead to cancer.
2) Why is it difficult to detect it?
Oesophageal cancer is very difficult to detect because early symptoms are non-specific and common, such as heartburn. By the time specific symptoms appear, such as difficulty and pain with swallowing, the disease is at a later stage. As a result only 20 per cent of patients are eligible for treatment that can cure their cancer and 80 per cent of patients are referred for palliative treatment, medical care that is aimed at controlling the disease and alleviating symptoms. The long-term survival rate is just 13 per cent for oesophageal cancer.
3) How is it currently diagnosed?
The diagnostic test for oesophageal cancer is an endoscopy. This is a procedure where the inside of the body is examined using a probe with a light source and video camera at the end via the mouth and down the gullet. This is an invasive and expensive test that can also lead to complications such as tearing of an organ and infections. Only two per cent of patients who are referred for an endoscopy by GPs are diagnosed with oesophageal cancer.
4) Can you tell me a bit more about your cancer breath test?
We have devised a cancer breath test to help diagnose oesophageal and gastric cancer. The test is 90 per cent accurate and provides results in minutes, which can take up to four to six hours to process using other methods. To take the test, patients breathe into a device similar to a breathalyser which is connected to a bag. The test looks for chemical compounds in exhaled breath that are unique to patients with oesophageal and gastric cancer. In our first clinical trial at Imperial College Healthcare NHS Trust in 2011 to 2013 we found that the test could discriminate between malignant and benign oesophageal cancer in over 200 patients.
5) How did you come up with devising a breath test?
There is some evidence which shows that dogs can sniff out cancer as they can smell minute odours known to be associated with many malignant cancers. We wanted to see whether we can replicate that with a device.
6) How can your breath test help patients?
The test can be used to diagnose patients with early non-specific symptoms which can give them more treatment options and could increase their chances of survival. It can also help reduce the number of invasive endoscopies carried out on patients. The test also has the potential to be used to screen patients who are most at risk of developing oesophageal cancer, for example men over the age of 60.
7) What are the next steps with your breath test?
We are currently running a larger study involving three other hospital trusts in London to see whether the breath test can produce similar results with a bigger group of patients. We have already recruited the patients for the trial from cancer centres throughout the UK. We hope to use the results from the trial to create a smaller sensor device that can be used by GPs to refer patients for further investigations.
For more information on oesophageal cancer contact Cancer Research's Cancer Information Nurses.
Article text (excluding photos or graphics) available under an Attribution-NonCommercial-ShareAlike Creative Commons license.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Maxine Myers
Communications Division

Contact details
Tel: +44 (0)7561 451 724
Email: maxine.myers@imperial.ac.uk
Show all stories by this author


Leave a comment
Your comment may be published, displaying your name as you provide it, unless you request otherwise. Your contact details will never be published.