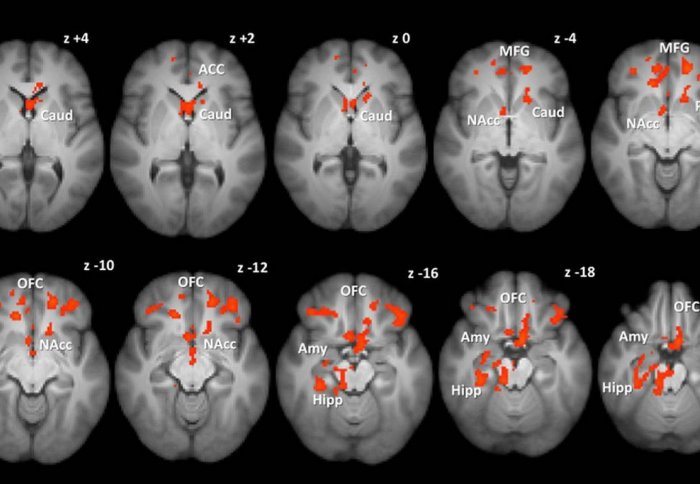
Certain brain areas had weaker responses to pictures of food in subjects who had gastric bypass operations.

Gastric bypass surgery changes how the brain responds to food, reducing not only hunger but also the drive to eat for pleasure, a study has found.
The research, published in the journal Gut, helps to explain why gastric bypass patients lose more weight over the long term than those who undergo a gastric band operation.
Weight loss surgery is the most effective treatment for obesity and its associated health problems. Over 20 years, people who undergo gastric bypass surgery lose on average 25 per cent of their body weight, compared with 14 per cent for those who have a gastric band.
The gastric bypass procedure re-routes the digestive system past most of the stomach so that undigested food gets to the intestine much quicker, while a gastric band physically restricts the size of the stomach so individuals feel full.
Previous studies in animals and humans have shown that those who undergo a gastric bypass tend to shift away from eating high-fat and sweet foods. However the effect of different types of weight loss surgery on the brain that may be responsible for changes in food preference has not been explored until now.
This may have important implications for the way we treat patients with obesity and could help pave the way for a more personalised approach when deciding on the choice of bariatric procedure.
– Dr Tony Goldstone
MRC Clinical Sciences Centre
Using a scanning technique called functional magnetic resonance imaging (fMRI), which measures brain activity by detecting changes in blood oxygen levels and flow, scientists studied 61 men and women who had lost weight from either a gastric bypass or gastric band surgery carried out on average eight to nine months previously, as well as a control group of unoperated participants. These three groups were of similar body weight.
They found marked differences in the brain’s response to food in patients after gastric bypass, compared to gastric band surgery. Patients who had gastric bypass had less activity in the brain’s reward regions when shown pictures of food compared with those who had gastric banding.
Patients after gastric bypass also rated high-calorie foods as less appealing to look at and less pleasant to eat, had healthier eating habits and ate less fat in their diet than patients after gastric banding or the unoperated control group. Both the gastric bypass and banding patients had similarly reduced hunger compared with the unoperated group, and the findings were not explained by differences in psychological traits between the surgical groups.
The researchers did not find conclusive evidence of what caused these changes, but they did observe several differences in the patients’ metabolism that could play a role. Levels of gut hormones called GLP-1 and PYY that make us feel full after a meal were higher in the gastric bypass group, as were levels of bile salts, which play a role in digestion.
Patients after gastric bypass also reported more intestinal discomfort and nausea after eating foods high in fat and sugar in the early months after the surgery than patients after banding, which may also be influencing what foods they want to eat. Further work by the researchers will focus on which of these factors may be influencing the brain’s response to food following bypass surgery.
Dr Tony Goldstone from the MRC Clinical Sciences Centre at Imperial College London, who led the study, said:
“It is well established that patients after gastric bypass lose more weight than after gastric band and we think this is because of the different physical changes made to the gut during surgery, which somehow have an effect on the drive to eat for pleasure. Both procedures reduce appetite and have health benefits including long-term weight loss and improvement or even complete resolution of type 2 diabetes. However, gastric bypass surgery appears to be more effective for weight loss and has a more profound effect on the way in which the brain responds to food.
“These findings emphasise that different bariatric procedures work in different ways to influence eating behaviour. This may have important implications for the way we treat patients with obesity and could help pave the way for a more personalised approach when deciding on the choice of bariatric procedure by taking the impact on food preferences and cravings into account."
Professor David Lomas, Chair of the MRC’s Population and Systems Medicine Board, which funded the research, said:
“Humans don’t just eat when they’re hungry – the pleasure and rewarding feelings we get from eating play a huge role in determining what kind of foods we eat, as well as how much. This work adds to a growing body of evidence supporting the role of the gut-brain interplay in controlling our eating behaviour. Being able to influence this relationship may in future play an important role in the development of non-surgical treatments for obesity.”
This research was supported by the Medical Research Council, Wellcome Trust, National Institute for Health Research, and Imperial College Healthcare Charity.
Based on a news release by the Medical Research Council.
Reference
Scholtz et al. ‘Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding’ Gut 2013. doi:10.1136/gutjnl-2013-305008
Supporters


Article text (excluding photos or graphics) available under an Attribution-NonCommercial-ShareAlike Creative Commons license.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Sam Wong
School of Professional Development

Contact details
Email: press.office@imperial.ac.uk
Show all stories by this author
Leave a comment
Your comment may be published, displaying your name as you provide it, unless you request otherwise. Your contact details will never be published.


Comments
Comments are loading...