
Schistosoma worms (the thinner female worm is tucked inside the larger male)

Scientists from Imperial have created a new test that could instantly detect the presence of the parasite schistosoma in a water supply.
The test uses a similar technology to a pregnancy test, and changes colour when the parasite is detected.
Details of the technology, which uses genetically modified versions of bacterial cells to detect the parasite, have just been published in the journal Scientific Reports.
Schistosomiasis is an enormous global health burden, and so we urgently need technologies to help prevent the spread of this disease
– Professor Paul Freemont
Study author
This test originated as an undergraduate project for the International Genetically Engineered Machine (iGEM) Competition by Imperial College students. The work was then continued by members of the synthetic biology group of Professor Paul Freemont in the Department of Medicine.
Although the researchers caution the work is at an early stage, they hope it could provide a cheap easy test for remote areas with limited resources.
The team used bacterial cells in the test as they can be freeze-dried and, in theory, transported around the world. Once they arrive at their destination they can be rehydrated with a drop of water, and ready to use within 24 hours.
Schistosomiasis is a disease caused by a parasitic worm that lives in tropical and sub-tropical areas, and is most commonly found in Africa. The parasite infects around 200 million people each year – many of them children - and can cause liver, kidney and bladder damage, infertility, and stunted growth.
The parasite infects snails in freshwater ponds, lakes or rivers – microscopic larvae are then released from these snails into the water where they infect people, by burrowing through their skin and into the body. These larvae then transform into worms inside the human body.
Identifying whether a water supply is infected is therefore key to stopping the disease. However, current tests can take a number of days, or require complex laboratory equipment, explained Dr Alex Webb, lead author of the research also from the Department of Medicine.
“The current tests need expensive equipment, or require samples to be sent to a lab for testing. Neither of these make it ideal for many of the regions of the world affected by this parasite.”
In the current work, the team genetically engineered two types of bacteria called Escherichia coli or Bacillus subtilis – both of which are found naturally in the human body. The bacteria were engineered to produce a type of ‘detector protein’ that signals the presence of the parasite. This detector protein is attached to a compound that changes colour when a particular chemical solution is added to it.
The idea behind the test is that a sample of, say, pond water is added to the bacterial cells, followed by the colour-changing chemical solution.
The detector protein, on the bacterial cells, contains a special code - called a recognition motif - that is only recognised by a parasite enzyme called elastase.
This enzyme is released by the parasite to breakdown human skin and gain entry to the body. If the parasite is present in a water sample, the elastase enzyme breaks the detector protein in half. This causes the colour-change compound to be lost, and so the sample doesn’t change colour when the chemical solution is added.
However, if the parasite is not in the water, the detector protein will remain intact, with the colour-change compound attached, and so the bacterial cells will turn red. This is shown below.

Dr Webb added they are working on another version that changes red in the presence of the parasite, and remains colourless when no parasite is present. The colour-change solution will also be integrated into the test, so that detecting the parasite simply involves dipping the test into a sample of water, with no need for extra solutions.
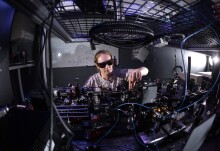
The work was conducted in the EPSRC Centre for Synthetic Biology and Innovation using the latest synthetic biology engineering techniques. The centre is part of Imperial’s synthetic biology hub - which also hosts the National UK Innovation and Knowledge Centre for Synthetic Biology (SynbiCITE). This is dedicated to the translation and commercialisation of synthetic biology research.
Professor Paul Freemont, Co-Director of the EPSRC Centre for Synthetic Biology and Innovation at Imperial, said this latest technology could hold great potential. “Schistosomiasis is an enormous global health burden - and we urgently need technologies to help prevent the spread of this disease. Although this technology is at an early stage, we now have proof of principal – and so can start developing this work further.”
"A protease-based biosensor for the detection of schistosome cercariae" by A. J. Webb et al. is published in Scientific Reports
Supporters

Article text (excluding photos or graphics) available under an Attribution-NonCommercial-ShareAlike Creative Commons license.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Kate Wighton
Communications Division

Contact details
Email: press.office@imperial.ac.uk
Show all stories by this author


Leave a comment
Your comment may be published, displaying your name as you provide it, unless you request otherwise. Your contact details will never be published.