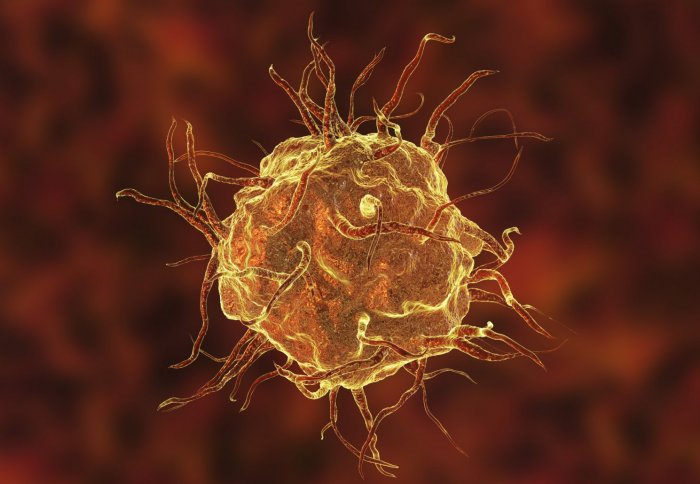
3D illustration of a macrophage cell

Scientists have found a way to 'program' immune cells to cause less damage to the body, by tapping into a 'broken' chemical pathway in inflammation.
The team, led by researchers at Imperial College London, Queen Mary University of London and Ergon Pharmaceuticals, believes the approach could offer new hope in the treatment of inflammatory conditions like arthritis, autoimmune diseases and sepsis.
In a study published this week in the journal Nature Communications, they explain how blocking a single enzyme enabled them to reprogram macrophages – the immune cells which are activated in inflammatory conditions – to calm their activity and reduce inflammation in rats and mice with human-like disease.
At the heart of the research is the Krebs cycle, a complex loop of reactions which cells use to feed on sugar and generate molecules of ATP, the universal energy currency for cells.
In recent years, research has shown that the usual pathway is interrupted in immune cells such as macrophages, leading to a broken Krebs cycle.
“In immune cells that have to fight invaders, the metabolism is diverted from its usual cycle to make compounds that fight microbes,” explained Dr Jacques Behmoaras, from the Department of Medicine at Imperial, who led the research.
Dr Behmoaras added: “What we have found is that there's an enzyme involved in this diversion of the usual cycle, which make immune cells produce these bacteria-killing compounds. If you block that enzyme, you block that specific branch of their metabolism, and make the cells cause less damage during inflammation.”
New findings
When ERG240 was given to mice with symptoms of rheumatoid arthritis, it reduced the inflammation in their joints by more than half while protecting the integrity of their joints.
– Dr Jacques Behmoaras
Department of Medicine
Using human macrophages, the researchers found that an enzyme called BCAT1 was pivotal in reprogramming macrophages. When the cells were activated – by exposing them to molecules found on the surface of bacteria – BCAT1 interfered with their usual metabolic pathways, and regulated another enzyme responsible for producing bacteria-killing chemicals.
They used an experimental compound called ERG240, developed by Ergon Pharmaceuticals, a small biotech company based in the US. ERG240 resembles the amino acid leucine, one of the building blocks of proteins, which is linked together by BCAT1. By flooding the cells with ERG240 they were able to jam up BCAT1 and block its action, so stopping the metabolism being diverted and ‘fixing’ the broken Krebs cycle. What’s more, the compound was effective in animal models of inflammation, without toxic side effects.
The team found that when ERG240 was given to mice with symptoms of rheumatoid arthritis, it reduced the inflammation in their joints by more than half while protecting the integrity of their joints. Similarly, in a rat model of severe kidney inflammation, they found that ERG240 improved kidney function by reducing the number of macrophages flooding into the affected tissue to cause inflammation.
Helping humans
Dr Behmoaras states that although the research is still at an early stage, there is potential for treating inflammatory conditions in patients by targeting the metabolic activity in immune cells. The team believes that BCAT1 works together with other key enzymes of the Krebs cycle, which could themselves provide targets for therapy.
I think this ability to regulate metabolism in cells could have an effect on many human diseases... This is a growing field of research with exciting discoveries ahead.
– Dr Jacques Behmoaras
Department of Medicine
However, one of the key challenges in developing a therapy would be in finding the balancing point: calming the immune cells enough such that they reduce inflammation, but enabling them to react to microbial invaders.
“I think this ability to regulate metabolism in cells could have an effect on many human diseases,” said Dr Behmoaras. “Manipulating cell activity in inflammatory diseases where macrophages have a role could have important therapeutic benefits."
“Our next step is to understand how other enzymes in the cycle are involved, to see if there is any possibility to block them and have similar effects. Understanding the complex metabolic circuits of these immune cells is a huge task. We will need to tackle this before we can manipulate cell activity and influence disease.
“This is a growing field of research with exciting discoveries ahead.”
The research was funded by the Medical Research Council and supported by Kidney Research UK.
"BCAT1 controls metabolic reprogramming in activated human macrophages and is associated with inflammatory diseases" by Papathanassiu, A.E. et al, published in Nature Communications, 12 July 2017.
Supporters


Article text (excluding photos or graphics) available under an Attribution-NonCommercial-ShareAlike Creative Commons license.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter

Ryan O'Hare
Communications Division

Contact details
Tel: +44 (0)20 7594 2410
Email: r.ohare@imperial.ac.uk
Show all stories by this author
Leave a comment
Your comment may be published, displaying your name as you provide it, unless you request otherwise. Your contact details will never be published.



Comments
Comments are loading...